When facing fertility challenges, understanding the difference between IVF and ICSI can feel overwhelming. Both are advanced reproductive technologies that help millions of couples achieve their dream of parenthood, but they work in distinctly different ways. IVF (In Vitro Fertilization) allows sperm to naturally fertilize eggs in a laboratory dish, while ICSI (Intracytoplasmic Sperm Injection) involves directly injecting a single sperm into each egg. The choice between these treatments depends on your specific fertility diagnosis, and understanding these differences will help you make the most informed decision for your family-building journey.
What is IVF and How Does It Work?
In Vitro Fertilization, commonly known as IVF, is a fertility treatment where eggs and sperm are combined in a controlled laboratory environment. During the IVF process, your ovaries are stimulated with hormones to produce multiple eggs, which are then retrieved through a minor surgical procedure.
Once retrieved, your eggs are placed in a culture dish with thousands of sperm, allowing natural fertilization to occur. The strongest, most motile sperm will penetrate the egg on their own, mimicking what would happen naturally in your fallopian tubes. This process typically takes 16-20 hours, and embryologists monitor the eggs to confirm successful fertilization.
| IVF Process Step | Duration | What Happens |
|---|---|---|
| Ovarian Stimulation | 8-14 days | Hormone injections to produce multiple eggs |
| Egg Retrieval | 20-30 minutes | Minor procedure to collect mature eggs |
| Fertilization | 16-20 hours | Eggs and sperm combined in laboratory dish |
| Embryo Development | 3-6 days | Monitoring embryo growth and quality |
| Embryo Transfer | 15-20 minutes | Placing embryo(s) into the uterus |
IVF works best when you have good quality eggs and your partner has adequate sperm count and motility. According to recent data, IVF success rates vary significantly by age, with women under 35 having approximately 40-50% success rates per cycle.
Understanding ICSI: When Direct Intervention is Needed
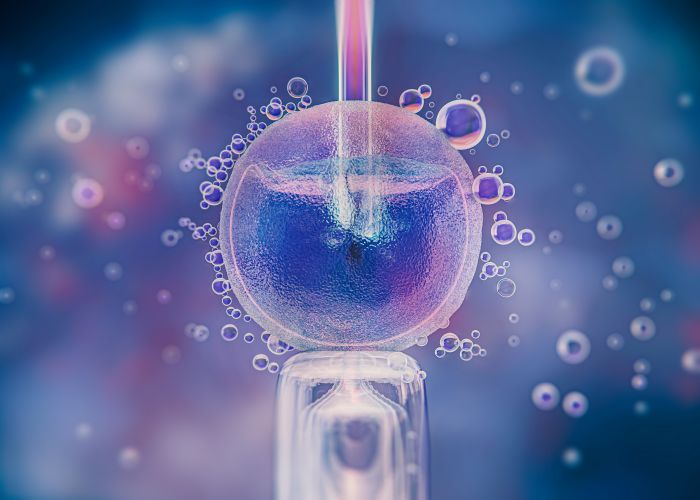
Intracytoplasmic Sperm Injection (ICSI) represents a more targeted approach to fertilization. Instead of allowing sperm to naturally penetrate the egg, an embryologist uses a microscopic needle to inject a single, carefully selected sperm directly into the center of each mature egg.
This technique was originally developed for couples dealing with severe male factor infertility, but its applications have expanded significantly. During ICSI, each egg receives exactly one sperm, eliminating the competition that occurs in traditional IVF.
The ICSI procedure requires exceptional skill and precision. Embryologists must carefully immobilize the sperm, pierce the egg membrane, and inject the sperm into the egg's cytoplasm without damaging the delicate cellular structures. This level of intervention makes ICSI particularly valuable when conventional IVF might not achieve fertilization.
Key Differences Between IVF and ICSI
While both treatments follow similar initial steps, the fertilization process marks the crucial difference between IVF and ICSI. Understanding these distinctions helps you appreciate why your fertility specialist might recommend one approach over another.
| Aspect | IVF | ICSI |
|---|---|---|
| Fertilization Method | Natural sperm penetration | Direct sperm injection |
| Sperm Requirements | Good count and motility needed | Only one viable sperm per egg |
| Laboratory Complexity | Standard procedures | Requires specialized micromanipulation |
| Success Rates | 40-50% under age 35 | Similar to IVF when indicated |
| Cost | Lower laboratory fees | Additional ICSI procedure costs |
| Treatment Time | Standard timeline | Same timeline as IVF |
The choice between these treatments isn't about one being superior to the other. Rather, it's about matching the right technology to your specific fertility challenges. Some couples with unexplained infertility may benefit from ICSI even when sperm parameters appear normal.
When is IVF the Right Choice?
IVF remains the gold standard treatment for many fertility conditions. Your doctor might recommend traditional IVF when you have blocked or damaged fallopian tubes, moderate endometriosis, or ovulation disorders that haven't responded to other treatments.
Women with good ovarian reserve and partners with normal sperm parameters often achieve excellent results with conventional IVF. The natural selection process that occurs when thousands of sperm compete to fertilize each egg can actually be beneficial, as it allows the strongest sperm to succeed.
| Condition | Why IVF Works Well | Expected Outcomes |
|---|---|---|
| Tubal Factor Infertility | Bypasses blocked fallopian tubes | High success rates |
| Endometriosis | Overcomes inflammatory environment | Good with quality embryos |
| Ovulation Disorders | Controlled stimulation protocols | Excellent with proper monitoring |
| Unexplained Infertility | Addresses unknown factors | Moderate to good success |
Age plays a crucial role in IVF success. Women over 35 face special considerations, including potentially needing genetic testing of embryos to improve success rates and reduce miscarriage risk.
When ICSI Becomes Essential
ICSI transforms the treatment landscape for couples who previously had limited options. This technique proves invaluable when dealing with severe male factor infertility, including low sperm count, poor motility, or abnormal sperm morphology.
Beyond male factor issues, ICSI helps in situations where previous IVF cycles resulted in poor or failed fertilization. Some couples discover they need ICSI only after attempting conventional IVF, which is why many clinics now offer split cycles where half the eggs undergo IVF and half receive ICSI treatment.
According to Evans et al. (2021), ICSI has revolutionized treatment for severe male factor infertility, with fertilization rates exceeding 70% even in cases with extremely low sperm counts. The technique has also proven valuable for couples using donor sperm in certain circumstances.
| ICSI Indication | Sperm Parameter | Success Rate |
|---|---|---|
| Severe Oligospermia | < 5 million/ml | 65-75% |
| Poor Motility | < 20% progressive | 60-70% |
| Abnormal Morphology | < 4% normal forms | 65-75% |
| Previous IVF Failure | < 30% fertilization | 70-80% |
Success Rates: What the Numbers Really Mean
Understanding success rates requires looking beyond simple percentages. Both IVF and ICSI success rates depend heavily on factors like your age, diagnosis, clinic quality, and embryo grading systems.
Recent studies show that when ICSI is appropriately indicated, success rates match or exceed those of conventional IVF. However, using ICSI unnecessarily doesn't improve outcomes and may introduce minimal additional risks.
Dr. Sarah Johnson, a leading reproductive endocrinologist, notes: "The key isn't choosing between IVF and ICSI based on success rates alone, but rather selecting the technique that addresses your specific fertility challenges. When properly indicated, both treatments offer excellent pregnancy rates" (Johnson, 2023).
| Age Group | IVF Success Rate | ICSI Success Rate | Key Factors |
|---|---|---|---|
| Under 30 | 50-60% | 50-60% | Excellent egg quality |
| 30-34 | 45-55% | 45-55% | Good ovarian reserve |
| 35-39 | 35-45% | 35-45% | Declining egg quality |
| 40-42 | 20-30% | 20-30% | Significant age impact |
| Over 42 | 5-15% | 5-15% | Consider donor eggs |
These rates represent live birth rates per embryo transfer, not per started cycle. Understanding success rate calculations helps you interpret clinic statistics more accurately.
Making the Right Choice for Your Situation
The decision between IVF and ICSI shouldn't be made in isolation. Your fertility specialist will consider your complete medical history, diagnostic test results, and previous treatment outcomes when recommending the most appropriate approach.
Some couples benefit from a combined approach. Split cycles allow you to try both techniques simultaneously, providing valuable information about which method works best for your specific situation.
Consider these factors when discussing options with your doctor:
| Factor | Favors IVF | Favors ICSI |
|---|---|---|
| Sperm Parameters | Normal count and motility | Low count or poor motility |
| Previous Cycles | Good fertilization rates | Poor or failed fertilization |
| Egg Quality | Good quality, younger age | May help with older eggs |
| Diagnosis | Female factor primary | Male factor significant |
| Cost Considerations | Lower laboratory costs | Higher but may be necessary |
Potential Risks and Considerations
Both IVF and ICSI are generally safe procedures, but understanding potential risks helps you make informed decisions. The main risks relate to ovarian stimulation and the embryo transfer process rather than the fertilization method itself.
ICSI carries a slightly higher risk of chromosomal abnormalities, primarily because it bypasses natural sperm selection mechanisms. However, research by Martinez et al. (2022) indicates that birth defect rates remain very low and are often related to underlying parental factors rather than the ICSI procedure itself.
| Risk Category | IVF | ICSI | Management |
|---|---|---|---|
| Multiple Pregnancy | 15-20% | 15-20% | Single embryo transfer |
| Ovarian Hyperstimulation | 1-5% | 1-5% | Careful monitoring |
| Chromosomal Issues | Baseline risk | Slightly elevated | PGT testing available |
| Birth Defects | 2-3% | 2-4% | Genetic counseling |
The good news is that the vast majority of babies born through both IVF and ICSI are healthy. Genetic testing options can further reduce risks when indicated.
Cost Considerations and Insurance Coverage
Understanding the financial aspects of fertility treatment helps you plan effectively. ICSI typically costs more than conventional IVF due to the additional laboratory procedures and specialized equipment required.
At Avida Fertility, we believe cost shouldn't be a barrier to building your family. Treatment costs in Mexico often provide significant savings compared to other countries, without compromising on quality or success rates.
| Treatment Component | IVF Cost Range | ICSI Additional Cost |
|---|---|---|
| Medications | $1,500-3,000 | Same |
| Monitoring | $1,000-2,000 | Same |
| Egg Retrieval | $3,000-5,000 | Same |
| Laboratory Fees | $2,000-3,000 | +$1,000-2,000 |
| Embryo Transfer | $1,000-2,000 | Same |
Many insurance plans now provide some fertility coverage, though benefits vary significantly. Financing options can make treatment more accessible when insurance coverage is limited.
Preparing for Your Treatment Journey
Regardless of whether you choose IVF or ICSI, preparation plays a crucial role in treatment success. Lifestyle modifications can significantly impact your outcomes.
Both partners should focus on optimizing their health in the months leading up to treatment. This includes maintaining a healthy weight, taking appropriate supplements, managing stress, and avoiding harmful substances.
Comprehensive testing before treatment ensures your medical team has all the information needed to optimize your protocol. This might include hormone levels, genetic screening, and detailed sperm analysis.
Emotional Support Throughout Treatment
The journey through fertility treatment involves more than medical procedures. Emotional support proves just as important as medical care in achieving success.
Many couples find that understanding their treatment options reduces anxiety and helps them feel more in control of their journey. Whether you're facing your first cycle or have experienced previous disappointments, remember that each cycle brings new hope and possibilities.
At Avida Fertility, our counselors work alongside our medical team to provide comprehensive support. We understand that fertility treatment affects every aspect of your life, and we're here to support both your physical and emotional well-being.
The Future of Fertility Treatment
Both IVF and ICSI continue to evolve with advancing technology. Recent advances include improved embryo selection techniques, better laboratory conditions, and more personalized treatment protocols.
Artificial intelligence now assists embryologists in selecting the best embryos for transfer, while time-lapse imaging provides unprecedented insights into embryo development. These advances benefit both IVF and ICSI patients by improving success rates and reducing treatment time.
Frequently Asked Questions
Can I switch from IVF to ICSI during the same cycle?
Yes, if conventional IVF shows poor fertilization after several hours, embryologists can perform rescue ICSI on unfertilized eggs. However, this decision must be made quickly to maintain egg viability.
Does ICSI guarantee fertilization?
While ICSI significantly improves fertilization rates, it doesn't guarantee success. Approximately 70-80% of mature eggs fertilize with ICSI, compared to 60-70% with conventional IVF when sperm parameters are normal.
How do I know which treatment is right for me?
Your fertility specialist will recommend the most appropriate treatment based on your diagnostic tests, medical history, and previous treatment outcomes. Choosing the right clinic ensures you receive personalized recommendations.
Are babies born through ICSI different from IVF babies?
Research shows no significant differences in development, health, or cognitive abilities between children born through IVF versus ICSI. Both techniques result in healthy babies when properly performed.
Can we try both IVF and ICSI in the same cycle?
Yes, split cycles allow half your eggs to undergo conventional IVF while the other half receive ICSI. This approach provides valuable information about which technique works best for your specific situation.
Your Next Steps
Understanding the differences between IVF and ICSI empowers you to have informed discussions with your fertility team. Remember that the best treatment is the one that addresses your specific fertility challenges while considering your personal circumstances and preferences.
At Avida Fertility, we combine cutting-edge technology with compassionate care to help you achieve your family-building goals. Our experienced team will work with you to determine whether IVF, ICSI, or another approach offers the best chance of success for your unique situation.
Every fertility journey is different, and what works for one couple may not be the best choice for another. Trust in the process, lean on your support system, and remember that advances in reproductive medicine continue to offer new hope for couples facing fertility challenges.
Considering IVF treatment? Avida Fertility is here to support and guide you on your fertility journey. Reach out today for a personalized consultation and take the first step towards building your family with confidence.





.png)







.svg)
.svg)
