The IVF process involves several carefully coordinated steps over 4-6 weeks, from initial ovarian stimulation through embryo transfer. Understanding each phase helps you feel more prepared and confident as you begin your fertility journey with personalized medical care.
What is IVF and When is it Recommended?
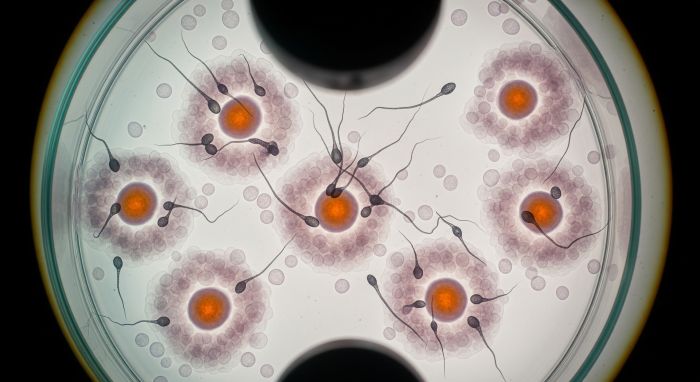
In Vitro Fertilization (IVF) is a fertility treatment where eggs are retrieved from your ovaries and fertilized with sperm in a laboratory setting. The resulting embryos are then transferred to your uterus to establish pregnancy.
Your doctor may recommend IVF for various conditions including blocked fallopian tubes, severe male factor infertility, endometriosis, unexplained infertility, or after unsuccessful IUI treatments. The decision depends on your specific diagnosis, age, and previous treatment history.
Complete IVF Process Timeline
The IVF process typically spans 4-6 weeks from start to finish. Here's what you can expect during each phase of your treatment cycle.
| Phase | Duration | Key Activities | What to Expect |
|---|---|---|---|
| Pre-treatment Preparation | 1-2 weeks | Birth control pills, baseline testing | Cycle synchronization and preparation |
| Ovarian Stimulation | 8-14 days | Daily hormone injections, monitoring | Multiple follicle development |
| Trigger Shot & Retrieval | 2-3 days | Final maturation, egg collection | Outpatient procedure under sedation |
| Fertilization & Culture | 3-6 days | Laboratory fertilization, embryo development | Daily updates on embryo progress |
| Embryo Transfer | 1 day | Embryo placement in uterus | Simple, usually painless procedure |
| Two-Week Wait | 10-14 days | Pregnancy test, progesterone support | Waiting period before results |
Step 1: Pre-Treatment Preparation and Testing
Before starting your IVF cycle, comprehensive testing ensures the best possible outcomes. Your medical team will review your fertility evaluation results and create a personalized treatment protocol.
During this phase, you may take birth control pills to synchronize your cycle and prepare your ovaries for stimulation. Baseline blood work and ultrasounds confirm you're ready to begin the active treatment phase.
According to Dr. Sarah Johnson from the American Society for Reproductive Medicine, "Proper preparation and individualized protocols significantly improve IVF success rates, particularly in patients over 35" (Johnson, 2023).
Step 2: Ovarian Stimulation Protocol
Ovarian stimulation is the foundation of successful IVF treatment. You'll receive daily hormone injections to encourage multiple eggs to mature simultaneously, rather than the single egg that develops naturally each month.
| Medication Type | Purpose | Administration | Duration |
|---|---|---|---|
| FSH (Follicle Stimulating Hormone) | Stimulate egg development | Daily injection | 8-12 days |
| LH (Luteinizing Hormone) | Support follicle maturation | Daily injection | Later in cycle |
| GnRH Antagonist | Prevent premature ovulation | Daily injection | 5-7 days |
| Trigger Shot (hCG) | Final egg maturation | Single injection | 36 hours before retrieval |
Your response to ovarian stimulation is carefully monitored through regular blood tests and ultrasounds. These appointments help your doctor adjust medication doses and determine the optimal timing for egg retrieval.
Step 3: Monitoring and Adjustments
Throughout the stimulation phase, you'll have frequent monitoring appointments every 2-3 days. These visits include blood work to measure hormone levels and transvaginal ultrasounds to assess follicle development.
Your medical team tracks several key indicators during monitoring visits. Estradiol levels reflect your ovarian response, while follicle measurements determine when eggs are ready for retrieval. This careful monitoring allows for real-time protocol adjustments to optimize your results.
Most patients develop 8-15 mature follicles during stimulation, though the exact number varies based on age, ovarian reserve, and individual response to medications.
Step 4: Trigger Shot and Final Preparation
When your follicles reach optimal size (typically 18-20mm), you'll receive a trigger shot containing hCG or Lupron. This injection completes the final maturation process and must be timed precisely 36 hours before your egg retrieval procedure.
The timing of your trigger shot is critical for successful egg collection. Your medical team will provide specific instructions about when to administer this injection, and it's essential to follow these directions exactly.
After your trigger shot, you'll have final pre-procedure instructions including fasting requirements and arrival time for your retrieval appointment.
Step 5: Egg Retrieval Procedure
Egg retrieval is an outpatient procedure performed under conscious sedation. Using transvaginal ultrasound guidance, your doctor will collect mature eggs from your ovaries using a thin needle.
| Aspect | Details |
|---|---|
| Procedure Duration | 20-30 minutes |
| Anesthesia | Conscious sedation |
| Recovery Time | 1-2 hours observation |
| Return to Normal Activities | Next day (avoid strenuous exercise) |
| Expected Discomfort | Mild cramping, similar to menstrual cramps |
The number of eggs retrieved varies based on your individual response to stimulation. While more eggs generally provide more opportunities, quality is equally important as quantity in determining success rates.
Your partner will provide a sperm sample on the same day, or previously frozen sperm will be thawed for the fertilization process.
Step 6: Fertilization and Embryo Development
Once your eggs are collected, the laboratory team begins the fertilization process. Depending on your specific situation, fertilization may occur through conventional IVF or ICSI (Intracytoplasmic Sperm Injection).
Your embryos are cultured in specialized incubators that maintain optimal conditions for development. The laboratory team monitors progress daily and provides updates on fertilization rates and embryo quality.
Embryo development follows predictable stages from fertilization through blastocyst formation. Your medical team will discuss whether to proceed with a Day 3 or Day 5 transfer based on embryo quality and quantity.
Step 7: Embryo Grading and Selection
Embryo grading helps determine which embryos have the highest potential for successful implantation. Your embryologist evaluates factors including cell number, fragmentation, and overall appearance.
For blastocyst transfers, embryo grading considers the inner cell mass, trophectoderm quality, and expansion level. Higher-grade embryos typically have better implantation rates, though lower-grade embryos can also result in successful pregnancies.
If you have multiple high-quality embryos, your doctor will discuss whether to transfer one or two embryos based on your age, previous treatment history, and personal preferences.
Step 8: Embryo Transfer Process
Embryo transfer is typically a simple, painless procedure that doesn't require anesthesia. Your doctor uses a thin catheter to place the selected embryo(s) directly into your uterus under ultrasound guidance.
The transfer procedure takes only a few minutes, and you can resume normal activities immediately afterward. Some doctors recommend a brief rest period, but bed rest isn't necessary for successful implantation.
Your endometrial lining should be adequately thick (typically 7mm or more) to support implantation. If your lining isn't optimal, your doctor may recommend a frozen embryo transfer in a subsequent cycle.
Step 9: Post-Transfer Care and Monitoring
After your embryo transfer, you'll begin progesterone supplementation to support the uterine lining and potential pregnancy. This medication is typically continued until 8-10 weeks of pregnancy if your cycle is successful.
The two-week wait between transfer and pregnancy testing can be emotionally challenging. It's normal to experience mild cramping, spotting, or other symptoms during this period, which don't necessarily indicate success or failure.
Your medical team will provide specific instructions about activity levels, medications, and warning signs to watch for during the waiting period.
Step 10: Pregnancy Testing and Follow-up
Approximately 10-14 days after your embryo transfer, you'll return for a blood pregnancy test (beta hCG). This test is more accurate than home pregnancy tests and can detect pregnancy earlier.
If your test is positive, you'll have repeat blood work to ensure hormone levels are rising appropriately. Your first ultrasound will typically occur around 6-7 weeks of pregnancy to confirm fetal heartbeat and proper development.
| Timeline | Milestone | What Happens |
|---|---|---|
| 10-14 days post-transfer | First beta hCG test | Initial pregnancy confirmation |
| 16-18 days post-transfer | Second beta hCG test | Hormone level progression check |
| 6-7 weeks pregnancy | First ultrasound | Fetal heartbeat confirmation |
| 8-10 weeks pregnancy | Graduation to OB care | Transition from fertility clinic |
IVF Success Rates and Factors
IVF success rates vary significantly based on age, diagnosis, and clinic-specific factors. According to the Society for Assisted Reproductive Technology, success rates by age show that women under 35 have approximately 40-50% live birth rates per cycle.
Dr. Michael Rodriguez from the International Federation of Fertility Societies notes, "Success rates continue to improve with advances in laboratory techniques, genetic testing, and personalized treatment protocols" (Rodriguez, 2023).
Factors that influence your individual success rates include ovarian reserve, sperm quality, uterine health, and previous pregnancy history. Your medical team will discuss realistic expectations based on your specific circumstances.
Managing Side Effects and Expectations
IVF medications can cause various side effects including bloating, mood changes, fatigue, and injection site reactions. Most side effects are temporary and resolve after treatment completion.
Ovarian hyperstimulation syndrome (OHSS) is a potential complication that occurs in 3-5% of IVF cycles. Your medical team monitors for OHSS symptoms and may adjust protocols to minimize risk.
Emotional support is equally important during IVF treatment. Many patients benefit from counseling, support groups, or stress-reduction techniques to manage the psychological aspects of fertility treatment.
Advanced IVF Technologies and Options
Modern IVF incorporates several advanced technologies to improve success rates. Preimplantation genetic testing (PGT) can identify chromosomally normal embryos, particularly beneficial for patients over 35 or those with recurrent pregnancy loss.
Time-lapse embryo monitoring systems allow continuous observation of embryo development without disturbing the culture environment. This technology helps identify the most viable embryos for transfer.
For patients with specific challenges, additional techniques like ICSI for unexplained infertility or assisted hatching may be recommended to optimize outcomes.
Financial Considerations and Planning
Understanding IVF treatment costs helps you plan financially for your fertility journey. Costs vary based on location, clinic, and specific treatments required.
Many patients require multiple IVF cycles to achieve pregnancy. Discussing package deals, financing options, and insurance coverage with your clinic's financial team helps you make informed decisions about your treatment plan.
International treatment options, such as those available in Mexico, can provide significant cost savings while maintaining high-quality medical care and advanced technology.
Preparing for Your IVF Journey
Successful IVF preparation involves both physical and emotional readiness. Optimizing your health through proper nutrition, regular exercise, and stress management can positively impact treatment outcomes.
Taking folic acid and other fertility supplements before starting treatment supports egg quality and early pregnancy development. Your doctor may recommend specific supplements based on your individual needs.
Creating a support system of family, friends, or fertility support groups provides emotional strength throughout your treatment journey.
Frequently Asked Questions About IVF
How long does the entire IVF process take?
A complete IVF cycle typically takes 4-6 weeks from the start of medications to pregnancy testing. However, preparation and testing may begin several weeks earlier.
Is IVF painful?
Most patients experience minimal discomfort during IVF. Daily injections may cause mild irritation, and egg retrieval can result in cramping similar to menstrual cramps. Pain medication helps manage any discomfort.
How many IVF cycles might I need?
The number of cycles varies greatly among patients. Some achieve pregnancy on their first attempt, while others may need multiple cycles. Your doctor will discuss realistic expectations based on your specific situation.
Can I work during IVF treatment?
Most patients continue working throughout IVF treatment with minimal disruption. You'll need time off for monitoring appointments and the egg retrieval procedure, but normal activities can typically continue.
What happens to unused embryos?
High-quality embryos not used in your fresh cycle can be frozen for future use. This provides additional opportunities for pregnancy without repeating the entire stimulation process.
Are there alternatives if IVF doesn't work?
If IVF is unsuccessful, options may include additional cycles with protocol modifications, donor eggs, donor sperm, or gestational surrogacy, depending on your specific circumstances.
Why Choose Avida Fertility for Your IVF Journey
At Avida Fertility, we combine cutting-edge technology with compassionate, personalized care. Our experienced team understands that every patient's journey is unique, and we tailor treatment protocols to optimize your individual success rates.
Our state-of-the-art laboratory facilities and advanced reproductive technologies ensure the highest standards of care throughout your treatment. We're committed to transparency, providing clear communication about your progress and realistic expectations at every step.
From your initial consultation through pregnancy achievement, our dedicated team supports you with expertise, empathy, and unwavering commitment to helping you build your family.
Considering IVF treatment? Avida Fertility is here to support and guide you on your fertility journey. Reach out today for a personalized consultation and take the first step towards building your family with confidence.




.png)







.svg)
.svg)
