If you're a smoker trying to conceive, you're not alone in wondering how cigarettes might be affecting your fertility journey. The good news is that quitting smoking can significantly improve your chances of getting pregnant, and your body begins healing faster than you might expect.
How Smoking Affects Your Fertility
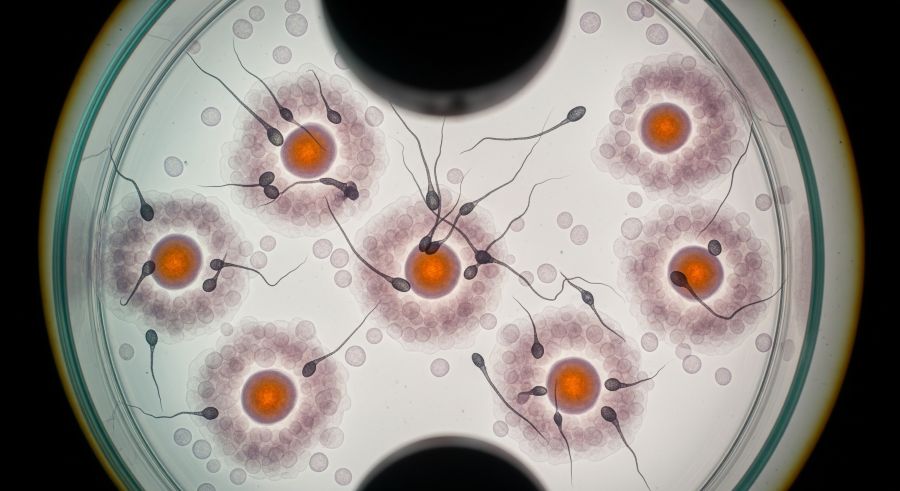
When you smoke, you're exposing your reproductive system to over 7,000 chemicals, including nicotine, carbon monoxide, and tar. These substances don't just affect your lungs—they travel through your bloodstream and directly impact your egg quality and reproductive organs.
For women, smoking accelerates the loss of eggs and can cause you to reach menopause 1-4 years earlier than non-smokers. The chemicals in cigarettes damage the DNA in your eggs, making them less likely to fertilize successfully or develop into healthy embryos.
| Smoking Impact | Women | Men |
|---|---|---|
| Fertility Reduction | Up to 60% decrease in conception rates | 23% reduction in sperm concentration |
| DNA Damage | Increased chromosomal abnormalities in eggs | Higher sperm DNA fragmentation |
| Hormone Disruption | Altered estrogen and progesterone levels | Reduced testosterone production |
| Treatment Success | Lower IVF success rates | Decreased fertilization rates |
Men aren't immune to smoking's effects either. Cigarettes reduce sperm count, decrease sperm motility, and increase the percentage of abnormally shaped sperm. According to research by Sharma et al. (2016), male smokers show a 23% reduction in sperm concentration and a 13% decrease in sperm motility compared to non-smokers.
The Science Behind Smoking and Reproductive Health
Understanding exactly how smoking damages your fertility can motivate you to quit and help you make informed decisions about your treatment timeline. The toxic chemicals in cigarettes create oxidative stress throughout your body, including in your reproductive organs.
Impact on Female Fertility
Smoking affects every aspect of female reproduction. The chemicals reduce blood flow to your reproductive organs, making it harder for your ovaries to function properly. Your fallopian tubes may also be damaged, increasing the risk of ectopic pregnancy.
Research shows that women who smoke have significantly lower AMH levels, indicating reduced ovarian reserve. This means you have fewer eggs available for conception, whether naturally or through fertility treatments.
Male Factor Fertility and Smoking
For men, smoking affects sperm production in the testicles and can damage sperm as they mature. The heat from smoking also raises scrotal temperature, which negatively impacts sperm quality. Additionally, smoking reduces the antioxidants that protect sperm from damage.
| Timeframe After Quitting | Female Recovery Benefits | Male Recovery Benefits |
|---|---|---|
| 2-12 weeks | Improved circulation to reproductive organs | Better sperm motility begins |
| 1-3 months | Hormone levels start normalizing | New, healthier sperm production cycle |
| 6-12 months | Significant improvement in egg quality | Optimal sperm parameters achieved |
| 1+ years | Fertility rates approach non-smoker levels | DNA fragmentation significantly reduced |
Recovery Timeline: When Your Body Heals
The moment you quit smoking, your body begins the healing process. While some damage may be permanent, many of smoking's effects on fertility are reversible with time and commitment to staying smoke-free.
Your circulation improves within just 2-12 weeks of quitting, which means better blood flow to your ovaries and uterus. For men, since sperm take about 74 days to fully mature, you'll see improvements in sperm quality within 2-3 months of quitting.
According to Dr. Practice Committee of the American Society for Reproductive Medicine (2018), women who quit smoking before starting fertility treatments have success rates that approach those of women who never smoked, especially if they quit at least one year before treatment.
Smoking's Impact on Fertility Treatments
If you're considering fertility treatments while still smoking, it's important to understand how cigarettes can affect your success rates. Smoking reduces the effectiveness of most fertility treatments and increases the risk of complications.
IVF and Smoking
Women who smoke during IVF treatment typically need higher doses of fertility medications and produce fewer eggs during stimulation. The eggs that are retrieved are often of lower quality, leading to fewer viable embryos.
Studies show that smoking women undergoing IVF have:
| Treatment Outcome | Smokers | Non-Smokers |
|---|---|---|
| Eggs Retrieved | 30% fewer on average | Standard response |
| Fertilization Rate | Reduced by 15-20% | Normal rates |
| Live Birth Rate | 50% lower per cycle | Standard success rates |
| Miscarriage Risk | 2x higher | Baseline risk |
Other Fertility Treatments
Smoking also affects the success of IUI treatments and reduces the effectiveness of fertility medications like Clomid and letrozole. Even if you conceive, smoking increases the risk of miscarriage, ectopic pregnancy, and pregnancy complications.
Secondhand Smoke and Fertility
Even if you don't smoke yourself, exposure to secondhand smoke can impact your fertility. The same toxic chemicals that affect smokers can also harm non-smokers who are regularly exposed to cigarette smoke.
If your partner smokes, their secondhand smoke exposure could be affecting your fertility journey. Creating a completely smoke-free environment in your home and car is essential for optimizing your chances of conception.
Strategies for Quitting Smoking Before Treatment
Quitting smoking is one of the most important steps you can take to improve your fertility. While it can be challenging, especially when you're already dealing with the stress of trying to conceive, the benefits for your fertility are immediate and significant.
Medical Support for Quitting
Talk to your fertility doctor about safe smoking cessation methods while trying to conceive. Some nicotine replacement therapies may be appropriate, while others should be avoided during fertility treatments or pregnancy attempts.
| Quit Method | Safety During TTC | Effectiveness | Considerations |
|---|---|---|---|
| Cold Turkey | Safest option | 3-5% success rate | Requires strong willpower |
| Nicotine Gum/Patches | Consult doctor first | 15-20% success rate | Lower nicotine exposure |
| Prescription Medications | Generally not recommended | 25-30% success rate | Potential pregnancy risks |
| Behavioral Therapy | Completely safe | 20-25% success rate | Addresses psychological aspects |
Timing Your Quit
Ideally, you should quit smoking at least 3-6 months before starting fertility treatments. This gives your body time to heal and improves your chances of treatment success. However, quitting at any point is beneficial—even quitting during treatment is better than continuing to smoke.
Supporting Your Partner Through Recovery
If your partner is the smoker, your support can make a significant difference in their quit success. Fertility challenges affect both partners, and working together to create a healthy environment improves outcomes for everyone.
Consider making lifestyle changes together, such as improving diet, increasing exercise, and managing stress. These changes not only support smoking cessation but also improve overall fertility for both partners.
Nutritional Support During Recovery
As your body heals from smoking, proper nutrition can accelerate recovery and improve your fertility. Focus on antioxidant-rich foods that help repair cellular damage caused by smoking.
Key nutrients for fertility recovery include folic acid, vitamin D, and omega-3 fatty acids. These nutrients support egg and sperm quality while helping your body eliminate toxins from smoking.
| Nutrient | Benefits for Recovery | Food Sources | Recommended Daily Amount |
|---|---|---|---|
| Vitamin C | Reduces oxidative stress | Citrus fruits, berries, leafy greens | 75-90mg |
| Vitamin E | Protects reproductive cells | Nuts, seeds, vegetable oils | 15mg |
| Folate | Supports DNA repair | Leafy greens, legumes, fortified grains | 400-800mcg |
| Zinc | Improves sperm quality | Oysters, meat, pumpkin seeds | 8-11mg |
When to Start Fertility Treatment After Quitting
The timing of when to start fertility treatment after quitting smoking depends on several factors, including your age, how long you've been trying to conceive, and any other fertility factors you may have.
If you're under 35 and have been trying to conceive for less than a year, your doctor may recommend waiting 6-12 months after quitting before starting treatment. This allows your body maximum time to recover and can improve your treatment success rates.
However, if you're over 35 or have been trying for more than a year, your fertility specialist may recommend starting treatment sooner while supporting your smoking cessation efforts. Age-related fertility decline means that waiting too long might not be in your best interest.
Success Stories and Hope
Many couples who quit smoking go on to have successful pregnancies, both naturally and through fertility treatments. Your past smoking history doesn't define your fertility future—what matters most is the healthy choices you make moving forward.
At Avida Fertility, we've seen countless patients improve their treatment outcomes after quitting smoking. Our comprehensive approach includes not just advanced fertility treatments, but also support for the lifestyle changes that can make the biggest difference in your success.
Frequently Asked Questions
How long after quitting smoking will my fertility improve?
You'll start seeing improvements in circulation and hormone levels within 2-12 weeks of quitting. For optimal fertility recovery, most doctors recommend waiting 3-6 months after quitting before starting fertility treatments, though some benefits begin immediately.
Can vaping affect fertility the same way as smoking?
Yes, vaping can negatively impact fertility. While e-cigarettes may contain fewer toxic chemicals than traditional cigarettes, they still contain nicotine and other substances that can harm egg and sperm quality. It's best to avoid all nicotine products when trying to conceive.
Will my IVF success rates be the same as a non-smoker after I quit?
With enough time smoke-free, your IVF success rates can approach those of women who never smoked. Most studies show significant improvement after 6-12 months of being smoke-free, with the best outcomes seen in women who quit at least one year before treatment.
Should both partners quit smoking for fertility treatment?
Absolutely. Both male and female fertility are affected by smoking. Since fertility is a team effort, both partners should quit smoking to optimize your chances of conception and ensure the healthiest possible pregnancy.
What if I've been smoking for many years—is it too late?
It's never too late to quit smoking for your fertility. While some effects of long-term smoking may be permanent, many aspects of fertility recover surprisingly quickly after quitting. Even women who have smoked for decades can see improvements in their fertility within months of quitting.
Moving Forward with Confidence
Quitting smoking is one of the most powerful steps you can take to improve your fertility, whether you're trying to conceive naturally or preparing for fertility treatment. While the process can be challenging, remember that every day without cigarettes is helping your body heal and improving your chances of building the family you dream of.
Your fertility journey may have brought you to this realization about smoking's impact, but it's also brought you to a place where you can make positive changes that will benefit not just your fertility, but your overall health for years to come.
At Avida Fertility, we understand that making lifestyle changes while dealing with fertility challenges can feel overwhelming. Our team is here to support you through every aspect of your journey, from choosing the right treatment to making the lifestyle changes that can improve your success.
Considering IVF treatment? Avida Fertility is here to support and guide you on your fertility journey. Reach out today for a personalized consultation and take the first step towards building your family with confidence.





.png)







.svg)
.svg)
