Choosing between artificial insemination and IVF can feel overwhelming when you're trying to build your family. Both treatments offer hope, but understanding their differences, success rates, and which might work best for your unique situation is crucial for making an informed decision about your fertility journey.
Understanding Artificial Insemination and IVF: The Basics
When you're facing fertility challenges, you'll likely encounter two primary treatment options: artificial insemination and in vitro fertilization (IVF). These treatments represent different approaches to helping you achieve pregnancy, each with distinct processes and applications.
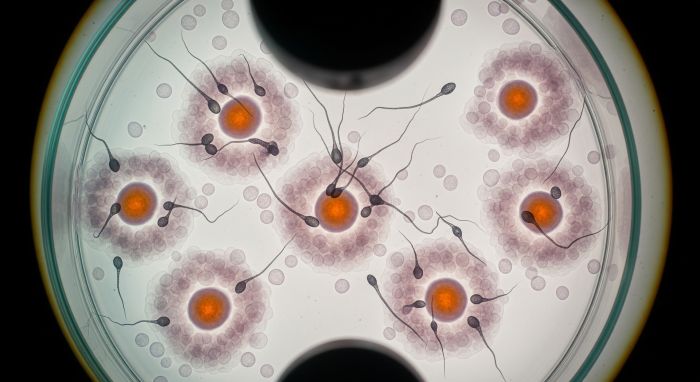
Artificial insemination, also known as intrauterine insemination (IUI), involves placing specially prepared sperm directly into your uterus around the time of ovulation. This procedure bypasses potential barriers in the cervix and gives sperm a head start in reaching your egg.
IVF, on the other hand, is a more complex process where your eggs are retrieved from your ovaries, fertilized with sperm in a laboratory setting, and then the resulting embryos are transferred back into your uterus. This treatment gives medical professionals greater control over the fertilization process.
Key Differences Between Artificial Insemination and IVF
The fundamental differences between these treatments extend beyond their basic procedures. Understanding these distinctions will help you grasp which approach might be more suitable for your specific fertility challenges.
| Aspect | Artificial Insemination (IUI) | In Vitro Fertilization (IVF) |
|---|---|---|
| Complexity | Less invasive, simpler procedure | More complex, multi-step process |
| Location of Fertilization | Inside your fallopian tubes (natural) | Laboratory setting (controlled) |
| Medication Requirements | Minimal to moderate hormone stimulation | Extensive hormone protocols |
| Monitoring Intensity | Basic cycle monitoring | Frequent ultrasounds and blood tests |
| Treatment Duration | 2-3 weeks per cycle | 4-6 weeks per cycle |
| Anesthesia Required | None | Yes, for egg retrieval |
The choice between these treatments often depends on your specific diagnosis, age, and previous treatment history. For single mothers by choice, both options can be effective depending on individual circumstances.
Success Rates: What You Can Realistically Expect
Success rates vary significantly between artificial insemination and IVF, and understanding these differences is crucial for setting realistic expectations. According to recent data from the American Society for Reproductive Medicine, IUI success rates typically range from 10-20% per cycle for women under 35, while IVF success rates are generally higher, ranging from 40-50% per cycle for the same age group.
| Age Group | IUI Success Rate per Cycle | IVF Success Rate per Cycle |
|---|---|---|
| Under 35 | 15-20% | 40-50% |
| 35-37 | 10-15% | 35-40% |
| 38-40 | 8-12% | 25-30% |
| Over 40 | 5-8% | 15-20% |
These rates can vary based on your specific fertility diagnosis. For example, if you have unexplained infertility, IUI might be surprisingly effective as a first-line treatment. However, if you have blocked fallopian tubes or severe male factor infertility, IVF would likely be more appropriate from the start.
When Artificial Insemination Is Recommended
Artificial insemination serves as an excellent first-line treatment for many fertility challenges. Your doctor might recommend IUI if you have unexplained infertility, mild male factor issues, or cervical factor infertility. This treatment is also commonly used with donor sperm for single women or couples with severe male factor infertility.
The procedure works best when your fallopian tubes are open and healthy, and when sperm quality meets certain minimum standards. Even with lower sperm counts, IUI can sometimes be effective because the sperm preparation process concentrates the healthiest sperm.
Many couples appreciate that IUI allows fertilization to occur naturally within your body, maintaining the natural selection process that happens in your fallopian tubes. The treatment is also less physically and emotionally demanding than IVF, making it an attractive option for those just beginning their fertility journey.
When IVF Becomes the Better Choice
IVF becomes the recommended treatment when artificial insemination is unlikely to be successful or when you've already tried multiple IUI cycles without success. Most fertility specialists recommend considering IVF after 3-4 unsuccessful IUI attempts, though this timeline can vary based on your age and specific circumstances.
Certain conditions make IVF the clear first choice. If you have blocked or damaged fallopian tubes, severe endometriosis, or significant male factor infertility requiring ICSI (intracytoplasmic sperm injection), IVF offers the best chance of success.
IVF also provides additional options that aren't available with IUI, such as preimplantation genetic testing (PGT) to screen embryos for genetic abnormalities. This can be particularly valuable if you're over 35 or have a history of genetic conditions.
Cost Considerations and Financial Planning
The financial aspect of fertility treatment is a significant consideration for most couples. Artificial insemination typically costs much less per cycle than IVF, but you may need multiple cycles to achieve success. A single IUI cycle might cost between $500-$1,500, while IVF can range from $10,000-$15,000 per cycle.
| Treatment | Cost per Cycle | Average Cycles Needed | Total Expected Investment |
|---|---|---|---|
| IUI | $500-$1,500 | 3-6 cycles | $1,500-$9,000 |
| IVF | $10,000-$15,000 | 1-3 cycles | $10,000-$45,000 |
When considering costs, it's important to factor in the cumulative success rates over multiple cycles. While IVF has a higher upfront cost, its higher success rate per cycle might make it more cost-effective in the long run, especially if you're over 35 or have been trying to conceive for an extended period.
Many financing options are available to help make treatment more accessible, including payment plans, fertility loans, and insurance coverage in some cases.
Physical and Emotional Demands
The physical and emotional demands of these treatments differ significantly. IUI involves minimal physical discomfort, with the actual insemination procedure taking just a few minutes and feeling similar to a routine pelvic exam. You might experience mild cramping afterward, but most women return to normal activities immediately.
IVF requires a more substantial physical and emotional commitment. The ovarian stimulation phase involves daily hormone injections for 8-12 days, frequent monitoring appointments, and potential side effects like bloating, mood swings, and fatigue. The egg retrieval procedure, while brief, requires sedation and a day of rest.
Emotionally, both treatments can be challenging, but IVF's intensity and higher stakes often create more stress. Having strong emotional support and coping strategies is crucial regardless of which treatment you choose.
Treatment Timelines and Scheduling
Understanding the timeline for each treatment helps you plan both personally and professionally. IUI cycles closely follow your natural menstrual cycle, with monitoring beginning around day 3 of your cycle and insemination occurring around day 14-16.
IVF requires more intensive scheduling. After initial testing and protocol planning, you'll begin hormone stimulation, typically requiring monitoring appointments every 2-3 days. The entire process from stimulation start to pregnancy test takes about 4-6 weeks.
| Treatment Phase | IUI Timeline | IVF Timeline |
|---|---|---|
| Initial Monitoring | Days 3-5 of cycle | Days 1-3 of cycle |
| Stimulation Period | 5-7 days (if used) | 8-12 days |
| Procedure Day | Day 14-16 of cycle | Day 12-16 for retrieval |
| Transfer/Insemination | Same day as procedure | 3-5 days after retrieval |
| Pregnancy Test | 14 days post-procedure | 9-12 days post-transfer |
Age-Related Considerations
Your age significantly impacts the success of both treatments, but the effect is more pronounced with IUI. As you age, egg quality declines, making natural fertilization in the fallopian tubes less likely to result in a healthy pregnancy.
For women under 35 with good ovarian reserve, IUI can be an excellent starting point. However, if you're over 40, your fertility specialist might recommend moving directly to IVF to maximize your chances of success while preserving your emotional and financial resources.
IVF offers the advantage of being able to assess embryo quality before transfer and, with PGT testing, can identify chromosomally normal embryos, which becomes increasingly important as maternal age increases.
Male Factor Considerations
Male fertility factors play a crucial role in determining which treatment is most appropriate. Comprehensive male fertility testing should always be completed before choosing a treatment path.
IUI can be effective for mild male factor infertility, as the sperm preparation process concentrates the healthiest sperm and places them directly in the uterus. However, if sperm count, motility, or morphology are severely compromised, IVF with ICSI becomes necessary.
Improving sperm quality through lifestyle changes and supplements can enhance the success of either treatment, but the improvements may take 2-3 months to become apparent due to the sperm production cycle.
Special Circumstances and Advanced Options
Certain situations require specialized approaches that favor one treatment over another. LGBTQ+ couples often start with IUI using donor sperm, as it's less invasive and more affordable for initial attempts.
If you have a history of recurrent pregnancy loss, your doctor might recommend IVF with PGT testing to screen embryos for genetic abnormalities before transfer. Similarly, if you're considering using donor eggs, IVF is the only viable option.
For couples dealing with both male and female fertility factors, IVF often provides the comprehensive approach needed to address multiple issues simultaneously.
Making Your Decision: Key Questions to Consider
Choosing between artificial insemination and IVF requires careful consideration of multiple factors. Start by discussing these key questions with your fertility specialist:
How long have you been trying to conceive, and what diagnostic tests have revealed about your fertility? Your specific diagnosis heavily influences which treatment is most likely to succeed. Consider your age, ovarian reserve, and any male factor issues that have been identified.
What are your financial resources and insurance coverage? While IUI is less expensive per cycle, multiple cycles can add up. Sometimes investing in IVF upfront can be more cost-effective in the long run.
How do you feel about the physical and emotional demands of each treatment? Some couples prefer starting with the less invasive IUI approach, while others want to pursue the treatment with the highest success rate immediately.
What is your timeline for building your family? If you're hoping to have multiple children or are concerned about age-related fertility decline, these factors should influence your treatment choice.
Frequently Asked Questions
How many IUI cycles should I try before moving to IVF?
Most fertility specialists recommend trying 3-4 IUI cycles before considering IVF, though this can vary based on your age, diagnosis, and individual circumstances. Women over 38 might be advised to try fewer IUI cycles or move directly to IVF.
Can I do IVF if IUI didn't work?
Absolutely. Many couples successfully conceive with IVF after unsuccessful IUI cycles. Failed IUI cycles don't predict IVF failure, as these treatments address fertility challenges differently.
Which treatment is more successful for unexplained infertility?
For unexplained infertility, IUI is often tried first due to its lower cost and invasiveness. However, IVF typically has higher success rates per cycle. Your age and how long you've been trying to conceive should influence this decision.
Do I need different medications for IUI versus IVF?
Yes, the medication protocols differ significantly. IUI might use minimal stimulation or natural cycles, while IVF requires more intensive hormone protocols to stimulate multiple egg development. Understanding potential side effects of these medications is important for planning.
Can I switch from IUI to IVF mid-cycle?
Generally, no. These treatments require different preparation and protocols. However, if you respond exceptionally well to IUI stimulation medications and produce many eggs, your doctor might discuss converting the cycle to IVF with egg retrieval.
The Avida Fertility Advantage
At Avida Fertility, we understand that choosing between artificial insemination and IVF is one of the most important decisions you'll make on your fertility journey. Our experienced team provides personalized care that considers not just your medical history, but your emotional needs, financial situation, and family-building goals.
Our state-of-the-art laboratory and advanced techniques ensure you receive the highest quality care regardless of which treatment path you choose. We believe in transparent communication, helping you understand your options fully so you can make informed decisions about your fertility treatment.
From choosing the right clinic to navigating the emotional aspects of treatment, we're here to support you every step of the way. Our success rates reflect our commitment to excellence, and our compassionate approach ensures you feel supported throughout your journey.
Remember, there's no universally "right" choice between artificial insemination and IVF. The best treatment is the one that aligns with your specific medical needs, personal preferences, and life circumstances. With proper guidance and support, both treatments can help you achieve your dream of building a family.
Considering fertility treatment? Avida Fertility is here to support and guide you on your fertility journey. Reach out today for a personalized consultation and take the first step towards building your family with confidence.





.png)




.svg)
.svg)
