Stress affects your fertility more than you might realize. When you're trying to conceive, the pressure and anxiety can create a cycle that impacts your hormones, ovulation, and overall reproductive health. Understanding this connection empowers you to take control of both your stress levels and your fertility journey.
Understanding the Stress-Fertility Connection
Your body doesn't distinguish between different types of stress. Whether you're dealing with work pressure, relationship challenges, or the emotional weight of trying to conceive, your body responds the same way. This response directly affects your reproductive system in ways that can make conception more difficult.
When you experience stress, your body releases cortisol, often called the "stress hormone." High cortisol levels can disrupt the delicate balance of reproductive hormones that control your menstrual cycle and ovulation. This disruption can lead to irregular periods, delayed ovulation, or even missed cycles entirely.
The hypothalamic-pituitary-adrenal (HPA) axis, which controls your stress response, also influences the hypothalamic-pituitary-gonadal (HPG) axis that regulates reproduction. When one system is overactive, it can suppress the other, creating a biological conflict between managing stress and maintaining fertility.
| Stress Response | Impact on Fertility |
|---|---|
| Elevated cortisol levels | Disrupts hormone balance |
| Increased adrenaline | Reduces blood flow to reproductive organs |
| Chronic inflammation | Affects egg and sperm quality |
| Sleep disruption | Interferes with hormone production |
| Changes in appetite | Impacts nutritional status for conception |
How Stress Affects Female Fertility
For women, stress can significantly impact every aspect of the reproductive process. Your menstrual cycle depends on a precise sequence of hormonal signals, and stress can disrupt this delicate timing at multiple points.
Chronic stress can delay or prevent ovulation by interfering with the release of gonadotropin-releasing hormone (GnRH) from your hypothalamus. Without proper GnRH signaling, your pituitary gland doesn't release the luteinizing hormone (LH) and follicle-stimulating hormone (FSH) needed for ovulation.
Research shows that women with higher stress levels often have longer menstrual cycles and are more likely to experience anovulatory cycles, where no egg is released. This makes natural conception impossible during those cycles.
Stress also affects the quality of your cervical mucus, which plays a crucial role in helping sperm reach and fertilize an egg. High stress levels can make cervical mucus less hospitable to sperm, reducing the chances of successful fertilization.
Additionally, chronic stress can impact the implantation process. Even if fertilization occurs, elevated cortisol levels can affect the uterine lining's ability to support a developing embryo, potentially leading to early pregnancy loss.
Stress and Male Fertility
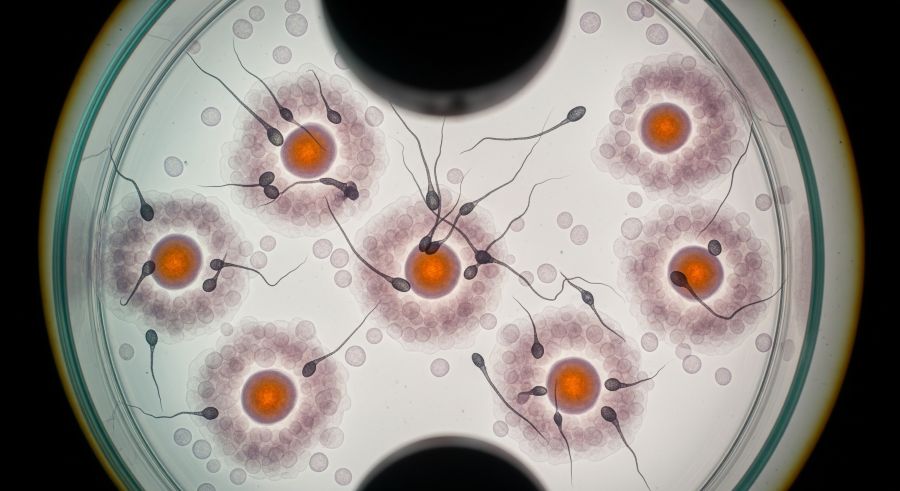
Men aren't immune to stress-related fertility issues. Chronic stress can significantly impact sperm production, quality, and function in several ways that directly affect conception chances.
Stress affects testosterone production, which is essential for healthy sperm development. When cortisol levels remain elevated, testosterone production decreases, leading to reduced sperm count and motility. This hormonal imbalance can persist for months, as sperm take approximately 74 days to fully develop.
According to Lynch et al. (2014), men experiencing high levels of psychological stress showed significant decreases in sperm concentration, motility, and normal morphology compared to men with lower stress levels. The study found that stress-related changes in sperm parameters could persist for several months after the stressful period ended.
| Stress Impact on Men | Effect on Sperm | Timeline for Recovery |
|---|---|---|
| Reduced testosterone | Lower sperm count | 3-4 months |
| Increased oxidative stress | DNA fragmentation | 2-3 months |
| Poor lifestyle choices | Decreased motility | 2-4 months |
| Sleep disruption | Abnormal morphology | 3-6 months |
Stress also increases oxidative stress in the body, which can damage sperm DNA and reduce fertilization potential. This oxidative damage affects not only the ability of sperm to reach and penetrate an egg but also the genetic integrity of the embryo if fertilization does occur.
The Fertility Treatment Stress Cycle
Ironically, fertility treatments themselves can become a significant source of stress, creating a challenging cycle that many couples face. The emotional, physical, and financial demands of fertility treatments can intensify the very stress that may be contributing to fertility challenges.
The uncertainty of treatment outcomes, the invasive nature of procedures, and the time commitment required can all contribute to increased anxiety levels. Many patients report feeling like their lives revolve around treatment schedules, monitoring appointments, and waiting for results.
This treatment-related stress can actually impact the success of fertility interventions. Studies have shown that women with higher anxiety levels during IVF treatment may have lower pregnancy rates, though the exact mechanisms aren't fully understood.
The financial stress of fertility treatments adds another layer of complexity. Concerns about treatment costs, insurance coverage, and the potential need for multiple cycles can create ongoing anxiety that affects your overall well-being and potentially your treatment outcomes.
Physiological Mechanisms Behind Stress-Induced Infertility
Understanding the biological pathways through which stress affects fertility can help you appreciate why stress management is such an important part of fertility care. The connection isn't just psychological – it's deeply rooted in your body's physiological responses.
The primary mechanism involves the HPA axis, which controls your body's stress response. When activated by chronic stress, this system releases cortisol and other stress hormones that can suppress the HPG axis responsible for reproduction. This suppression occurs at multiple levels, from the brain's hormone-releasing centers to the ovaries and testes themselves.
Chronic stress also triggers inflammatory responses in your body. This inflammation can affect egg quality, sperm function, and the uterine environment needed for implantation. Inflammatory markers like interleukin-6 and tumor necrosis factor-alpha have been found to be elevated in people experiencing fertility challenges.
Blood flow changes represent another important mechanism. Stress causes blood vessels to constrict, potentially reducing blood flow to reproductive organs. This reduced circulation can affect ovarian function, uterine lining development, and testicular sperm production.
| Physiological System | Stress Response | Fertility Impact |
|---|---|---|
| Hormonal | Elevated cortisol, reduced sex hormones | Disrupted ovulation, reduced sperm production |
| Immune | Chronic inflammation | Poor egg/sperm quality, implantation issues |
| Vascular | Reduced blood flow | Compromised reproductive organ function |
| Metabolic | Altered glucose and insulin levels | Hormonal imbalances affecting fertility |
Evidence-Based Stress Reduction Strategies
Fortunately, research has identified several effective approaches for managing stress during your fertility journey. These strategies can help break the stress-infertility cycle and potentially improve your chances of conception, whether naturally or through fertility treatments.
Mind-body interventions have shown particular promise in fertility care. Techniques like meditation, yoga, and progressive muscle relaxation can help activate your body's relaxation response, counteracting the effects of chronic stress. A study by Domar et al. (2011) found that women participating in mind-body programs had significantly higher pregnancy rates compared to control groups.
Cognitive-behavioral therapy (CBT) specifically designed for fertility challenges can help you develop coping strategies and change thought patterns that contribute to stress. This approach addresses both the practical and emotional aspects of fertility struggles, providing tools for managing anxiety and maintaining hope throughout treatment.
Regular exercise, when done in moderation, can be an excellent stress reducer. Physical activity helps metabolize stress hormones and releases endorphins that improve mood. However, excessive exercise can actually increase stress on your body, so finding the right balance is important for your fertility health.
Nutritional Support for Stress and Fertility
Your diet plays a crucial role in both stress management and fertility support. Certain nutrients can help your body better cope with stress while also supporting reproductive health. Understanding these connections can help you make dietary choices that benefit both your mental well-being and fertility potential.
B-vitamins, particularly B6, B12, and folate, are essential for neurotransmitter production and stress hormone regulation. These vitamins also play critical roles in DNA synthesis and cell division, making them important for both egg and sperm health. Folic acid supplementation is particularly important for women trying to conceive.
Omega-3 fatty acids have anti-inflammatory properties that can help counteract stress-induced inflammation. These healthy fats also support hormone production and may improve egg quality. Studies suggest that adequate omega-3 intake is associated with better fertility outcomes in both men and women.
Antioxidants like vitamin C, vitamin E, and selenium help protect reproductive cells from oxidative stress damage. This protection is especially important when chronic stress increases free radical production in your body. Foods rich in antioxidants can support both stress resilience and fertility.
| Nutrient | Stress Benefits | Fertility Benefits | Food Sources |
|---|---|---|---|
| Magnesium | Muscle relaxation, better sleep | Hormone regulation | Leafy greens, nuts, seeds |
| Vitamin D | Mood regulation | Hormone production | Fatty fish, fortified foods |
| Zinc | Immune function | Sperm quality, ovulation | Oysters, beef, pumpkin seeds |
| Iron | Energy production | Ovulatory function | Red meat, spinach, lentils |
Sleep Quality and Fertility Stress Management
Quality sleep is fundamental to both stress management and fertility health, yet it's often disrupted when you're dealing with fertility challenges. Understanding the connection between sleep, stress, and reproduction can help you prioritize rest as part of your fertility care plan.
During sleep, your body produces many of the hormones essential for reproduction, including growth hormone, which supports egg and sperm development. Sleep deprivation can disrupt this hormone production and increase cortisol levels, creating a double impact on fertility.
Poor sleep quality also affects your body's ability to manage stress effectively. When you're sleep-deprived, you're more likely to perceive situations as stressful and less able to cope with challenges. This can intensify the emotional aspects of fertility treatment and create additional stress.
The relationship between sleep and fertility is bidirectional – fertility stress can disrupt sleep, and poor sleep can worsen fertility challenges. Breaking this cycle requires intentional strategies for improving sleep hygiene and managing bedtime anxiety.
Professional Support and Counseling
Seeking professional support for fertility-related stress isn't a sign of weakness – it's a proactive step toward optimizing your chances of success. Mental health professionals who specialize in fertility can provide targeted strategies and support that general counseling might not address.
Fertility counselors understand the unique challenges you face, from the medical complexities of treatment to the social pressures surrounding parenthood. They can help you develop coping strategies specific to fertility stress, such as managing injection anxiety, dealing with treatment failures, or navigating relationship challenges that arise during fertility treatment.
Support groups, whether in-person or online, can provide valuable peer support and reduce feelings of isolation. Connecting with others who understand your experience can help normalize your feelings and provide practical tips for managing stress throughout treatment.
Some fertility clinics, including advanced centers like Avida Fertility, integrate mental health support into their treatment programs. This holistic approach recognizes that addressing psychological well-being is an important component of comprehensive fertility care.
Complementary Therapies for Fertility Stress
Many couples find that complementary therapies can be valuable additions to conventional fertility treatment, particularly for stress management. While these approaches shouldn't replace medical treatment, they can provide additional support for your overall well-being during fertility care.
Acupuncture has shown promise in fertility care, with some studies suggesting it may help reduce stress and improve treatment outcomes. The relaxation response triggered by acupuncture sessions can help counteract chronic stress, and some research indicates it may improve blood flow to reproductive organs.
Massage therapy can provide both physical and emotional benefits during fertility treatment. Regular massage can help reduce cortisol levels, improve circulation, and provide a dedicated time for relaxation and stress relief. Some fertility clinics offer specialized fertility massage techniques.
Herbal supplements and aromatherapy may also provide stress relief, though it's important to discuss any supplements with your fertility team to ensure they don't interfere with your treatment protocols. Some herbs can affect hormone levels or interact with fertility medications.
| Complementary Therapy | Stress Benefits | Considerations for Fertility Treatment |
|---|---|---|
| Acupuncture | Reduces cortisol, promotes relaxation | Generally safe, may complement IVF |
| Yoga | Combines movement and mindfulness | Avoid hot yoga, modify poses as needed |
| Massage | Muscle tension relief, improved circulation | Avoid deep abdominal massage during treatment |
| Meditation | Activates relaxation response | No contraindications, can be done anywhere |
Creating a Stress-Reduction Plan
Developing a personalized stress-reduction plan can help you feel more in control of your fertility journey and potentially improve your treatment outcomes. This plan should be realistic, sustainable, and tailored to your specific stressors and preferences.
Start by identifying your primary stress triggers related to fertility. These might include medical appointments, treatment procedures, financial concerns, or social situations. Understanding your specific stressors allows you to develop targeted coping strategies.
Build daily stress-management practices into your routine. This might include morning meditation, evening walks, journaling, or regular phone calls with supportive friends or family members. Consistency is more important than duration – even five minutes of daily stress relief can make a difference.
Plan for high-stress periods, such as during ovarian stimulation or while waiting for pregnancy test results. Having specific strategies ready for these times can help you navigate them more successfully.
When to Seek Additional Support
While some stress during fertility treatment is normal, there are times when professional intervention becomes important for both your well-being and your treatment success. Recognizing when you need additional support is an important part of self-care.
Consider seeking professional help if you're experiencing persistent anxiety that interferes with daily activities, depression that affects your motivation or energy levels, or relationship conflicts that seem related to fertility stress. These issues can all impact your treatment experience and potentially your outcomes.
Physical symptoms of chronic stress, such as persistent headaches, digestive issues, or sleep problems, also warrant attention. These symptoms can indicate that stress is affecting your overall health in ways that might impact fertility.
If you find yourself avoiding social situations, isolating from friends and family, or feeling hopeless about your fertility prospects, these are signs that additional support could be beneficial. Mental health support during fertility treatment isn't just about feeling better – it's about optimizing your chances of success.
Frequently Asked Questions
Can stress alone cause infertility?
While stress rarely causes infertility by itself, chronic stress can significantly impact fertility by disrupting hormone balance, affecting ovulation, and reducing sperm quality. Stress often compounds existing fertility challenges rather than being the sole cause.
How long does it take for stress reduction to improve fertility?
The timeline varies depending on the individual and the type of stress management approach used. Some benefits, like improved sleep and mood, may be noticed within weeks. However, changes in reproductive function may take 2-3 months to become apparent, as this reflects the time needed for new eggs and sperm to develop.
Will fertility treatments work if I'm stressed?
Fertility treatments can still be successful even when you're experiencing stress. However, managing stress may improve your treatment experience and potentially your outcomes. Many successful patients experience stress during treatment – the key is developing healthy coping strategies.
Should I delay fertility treatment until my stress is under control?
This depends on your individual situation, including your age, diagnosis, and the severity of your stress. It's best to discuss this with your fertility team, who can help you weigh the benefits of immediate treatment versus stress management. Often, stress management can be incorporated alongside treatment rather than delaying care.
Can my partner's stress affect our fertility treatment success?
Yes, stress can affect both partners' fertility. Male stress can impact sperm quality, while stress in either partner can affect the relationship dynamics and treatment adherence. Supporting each other's stress management is beneficial for both individual and couple well-being during fertility treatment.
Understanding the connection between stress and fertility empowers you to take an active role in managing both aspects of your health. While you can't eliminate all stress from your fertility journey, you can develop effective strategies for managing it in ways that support both your well-being and your reproductive goals.
Remember that seeking support for fertility-related stress is a sign of strength, not weakness. Whether through professional counseling, support groups, complementary therapies, or lifestyle changes, there are many effective ways to reduce stress and support your fertility journey.
Considering IVF treatment? Avida Fertility is here to support and guide you on your fertility journey. Reach out today for a personalized consultation and take the first step towards building your family with confidence.






.png)





.svg)
.svg)
